Re: Response to a Letter From the Canadian Pediatric Society and Alberta Medical Association to the Premier of Alberta
The Canadian Paediatric Society (CPS) and the Alberta Medical Association (AMA) recently sent a letter to the Premier of Alberta expressing their opposition to her proposed policy changes to pediatric gender medicine and the teaching of gender identity in schools. The letter ignores the recent systematic reviews of hormonal treatment for children and adolescents with gender dysphoria (GD), and the fact that the UK, Finnish, and Swedish national healthcare institutions all concluded, after systematic reviews, that there is insufficient evidence to determine that hormonal interventions for gender dysphoria in minors are safe. Your letter also misrepresents the scientific evidence on the risks of treatment.
Risk of Suicide
The letter claims that the proposed policies will “…lead to significant negative health outcomes, including increased risk of suicide and self-harm.” While it is true that many youth with gender dysphoria report elevated rates of suicidal thoughts, it is highly irresponsible to suggest that particular policies will lead to increased suicide risk, or alternately that providing gender affirming care will decrease it.
Suicidality is always the result of multiple factors. The rates of suicidality in youth with GD is higher than in youth without mental illness, but is similar to rates found in youth with other types of psychiatric morbidity (de Graaf et al., 2020). The assumption in the letter is that the GD is the cause of the suicidality. However, there is no way to prove causation, as suicidality is also correlated with the other types of mental illness often seen in youth with GD, such as depression, anxiety, eating disorders and complex trauma (Biggs, 2022).
There is no credible evidence that gender affirming care leads to reduced rates of suicidality. A recent systematic review of hormone therapy found that, “It was impossible to draw conclusions about the effects of hormone therapy on death by suicide.” (Baker et al., 2021, p. 12) Youth at risk of suicide need good general mental health care that considers all of their problems and does not focus on gender affirmation as the only way forward.
Furthermore, suicidality is known to be socially contagious (Martínez et al., 2023) and suicide prevention organizations have developed guidelines for responsible reporting on suicide which warn against providing simplistic explanations or portraying suicide as a means to an end (Sinyor et al., 2018). These guidelines are being flouted by advocates for gender affirming care who make inflammatory statements, based on questionable data, about suicide risk without considering how their rhetoric could affect vulnerable youth (Mohamed, 2024).
Gender Affirming Medical Care
The letter claims, “When it comes to gender-affirming medical care, current best practice shows that younger age and earlier pubertal stage at time of presentation has been associated with lower rates of mental health conditions.”
This statement and the supporting study mean something quite different from what the letter implies. The cross-sectional study found that children referred to gender clinics at younger ages had, at the time of initial assessment, fewer mental health conditions than older children (Sorbara et al., 2020). There is nothing in this study that supports the conclusion that treatment at a younger age actually led to improved mental health. Indeed, the study could support an approach to treat younger children with watchful waiting to see if their [gender] distress resolves naturally during puberty (Singh et al., 2021; Steensma et al., 2013).
The letter ignores the shifting international consensus around gender affirming care for young people. The Standard of Care of the World Professional Association for Transgender Health (Coleman et al., 2022), which the letter relies on, does not meet modern standards for a reliable clinical standard of care (Dahlen et al., 2021). Systematic reviews provide the highest level of evidence for the effectiveness of medical treatments and are the starting point for an evidenced-based standard of care. Finland, Sweden and the United Kingdom have conducted systematic evidence reviews for gender affirming care. They all found that the supporting evidence is poor quality and are leaning away from medicalization (Block, 2023a). Norway has also concluded the evidence of long term effects of gender affirming treatments for young people is insufficient (Block, 2023b) and Denmark has very recently begun significantly restricting hormone interventions for adolescents (SEGM, 2023). In January 2024, the Parliament of the Netherlands passed a motion asking the government to order an independent review of the pioneering “Dutch protocol” that uses puberty blockers and cross-sex hormones for gender-affirming care in children (Lane, 2024).
Puberty Blockers
The letter goes on to claim that, “Hormonal suppression is reversible and sex steroid production will resume if blockers are discontinued.” The letter cites the 8th edition of the WPATH Standard of Care in support of this proposition (Coleman et al., 2022).
While it is true that the immediate effect of blockers is temporary, this does not mean that they are reversible. Puberty blockers disrupt the production of hormones during a period in which children undergo critical developmental milestones. Once a developmental milestone is passed, the process cannot be fully reversed.
Puberty blockers have been approved for use in the treatment of precocious puberty where the drugs are stopped at the beginning of the normal window for puberty. Findings from studies of puberty suppression during precocious puberty cannot be extrapolated to their use during the normal, healthy, window for puberty as is the case with gender affirming care
Puberty is the period when bone density increases most rapidly. Disrupting puberty will slow the increase in bone density and it will only be partially made up if the patient proceeds to cross sex hormones. This can lead to increased risk of early onset osteoporosis (Biggs, 2021).
Puberty is also a critical milestone in brain development and sex hormones play a critical role in this process. There is very little research on the impact of puberty blockers on brain development but there are some studies which suggest that they could impact cognitive development and lead to a significant reduction in IQ (Baxendale, 2024).
Studies have found that almost all children who are started on puberty blockers at Tanner Stage 2 for gender dysphoria proceed to cross-sex hormones. This will almost certainly lead to permanent sterility (Stolk et al., 2023).
The letter claims that “adolescents who have sought and received hormonal suppression as part of a multidisciplinary approach to care report improved mental health and psychosocial functioning and lower odds of suicidal ideation” and cites in support a study by Dr. Jack Turban (Turban et al., 2020). This study has multiple methodological problems. It is based on a low quality online survey by an activist organization and it is unclear if the respondents understood what puberty blockers were, since a large majority reported having started after the age of 18 (Biggs, 2020).
Hormone Therapy
On the subject of gender affirming hormone therapy the letter claims that, “When GAHT is initiated appropriately for adolescents who desire this option, it has been associated with improved well-being and mental health, decreased suicidality, and decreased body dissatisfaction.”
The first question here is what “initiated appropriately” means. The letter suggests that GAHT is being initiated for adolescents “with marked and sustained gender diversity,” and “confirmed diagnosis of gender dysphoria or gender incongruence.” The initial Dutch study of hormonal treatment of young people used puberty suppression and hormonal treatment only for patients with a history of childhood onset gender dysphoria which worsened during puberty and with no comorbid mental health conditions (Abbruzzese et al., 2023).
Today, hormonal therapy is routinely prescribed for adolescents and young adults who did not experience gender related distress prior to puberty and who often present with significant mental issues and neurodevelopmental conditions such as autism spectrum disorder (Levine et al., 2022).
The letter claims that GAHT “has been associated with improved well-being and mental health, decreased suicidality, and decreased body dissatisfaction.” It cites, in support, a single study of 47 patients (Allen et al., 2019). Like many studies in this area, this study is of very low quality. The follow-up period was only 3 months and there was no control group. Therefore, it is not possible to say whether hormonal therapy actually contributed to the reported improvements in mental health or whether these improvements might have occurred naturally with the passage of time and from other, psychological and supportive treatments being given concurrently. The National Institute for Health Care and Excellence in the United Kingdom, examining the evidence in support for gender affirming hormones for children and adolescents, after systematic review, concluded that this study is of very low quality (National Institute for Health and Care Excellence, 2020).
Systematic reviews of hormonal therapy for adolescents have consistently found that the evidence supporting it is of such low quality that it would be irresponsible to link strong recommendations to this evidence (Block, 2023a). The World Health Organization recently stated that it would not be issuing guidelines for gender-affirming care for children and adolescents because the evidence base “…is limited and variable regarding the longer-term outcomes of gender affirming care for children and adolescents.” (World Health Organization, 2024)
Surgery
While surgeries on the reproductive organs are generally not performed before the age of majority, there is still significant cause for concern. The human brain does not reach full maturity until around the age of 25, when the prefrontal cortex that regulates risk assessment and long-term decision making, fully develops. While banning surgery on minors is prudent, there also need to be measures to ensure that young adults are being properly assessed and are giving proper informed consent (Levine, 2019; Levine et al., 2022). There is ample precedent for governments, in the public interest, to prohibit or regulate medical and surgical treatments offered to adults who are fully capable of informed consent.
Sexual Health Education
We agree that, “Comprehensive, evidence-based, medically accurate and age-appropriate sexual and reproductive health education has an overwhelming evidence base for its impact on positive health outcomes.” However, this is not currently being offered in many Alberta classrooms. Instead, students are being exposed to ideologically driven materials beginning at a young age, which are both misleading and harmful.
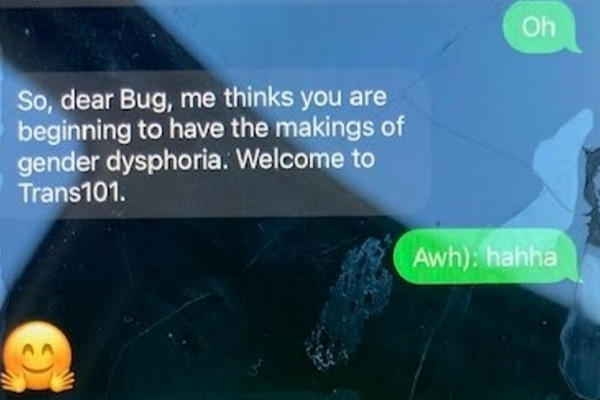
The current Alberta curriculum is based on the SOGI 123 program which makes sexual orientation and gender identity a central theme (SOGI 1 2 3 / Alberta, n.d.). The harm often starts with teaching tools such as the gender elephant or gender unicorn which indoctrinate children in the pseudo-scientific idea of sex and gender as a spectrum (Wright, 2021). At best, they are misinformed about a basic biological concept. At worst, they are left unable to distinguish between socially determined gender roles and sex, which may lead to gender confusion and cross-gender identification. SOGI 123 materials promote gender stereotypes and conflate sex and gender – for example by defining gay and lesbian as being sexually attracted to the same gender rather than the same sex. SOGI 123 may be particularly problematic for gay and lesbian adolescents who are typically gender non-conforming who may prematurely conclude that they are transgender and may feel that their same sex attraction is wrong.
Older children and teens are being exposed to books which describe and illustrate sexual acts in pornographic details. The book Let’s Talk About It is a particularly egregious example. It claims that sexually transmitted infections “aren’t as big of a deal as people make them out to be” and encourages teens to research sexual kinks by watching internet pornography (Right Side of HistoryTM️ [@xxclusionary], 2023). These kinds of materials contravene public health guidance which categorizes most sexually transmitted infections and sexual kinks that can lead to blood to blood or bodily fluid contact as high risk and inappropriate to be promoting to minors.
Conclusions
We agree with the statement that “medical decisions need to be made through informed and confidential discussions between healthcare professionals and the patient/family, guided by best-available evidence to support physical and mental well-being,” but this is not what is actually happening. Instead, as your letter reveals, pressure is being applied to make available serious medical interventions when the risk:benefit ratio cannot be properly assessed on the basis of the current evidence. Low-quality evidence is being leveraged to make assertions and even mislead the public about the safety and efficacy of these treatments and clinicians who question these assertions are being silenced. Families, even of quite young children, are being excluded from the decision-making process or pressured into compliance. Patients are not being properly informed of the potential risks of gender affirming care and there is no oversight to track outcomes and follow up with the patient population to assess safety or improve the quality of care. While political interference with medical decision making is generally undesirable, this is a case where there has been a serious failure in professional self-regulation, and therefore, some government action is necessary to correct course. The very reasonable recommendations of the current Alberta government are an appropriate and responsible step forward given the lack of quality evidence to support the types of recommendations the CPS and AMA seem to be comfortable promoting to Canadian families of vulnerable gender-questioning children and young people.
Sincerely,
Pamela Buffone, Canadian Gender Report
Dr Susan Bradley, Former Director, CAMH, Child and Adolescent Gender Identity Clinic
Roy Eappen MDCM, FRCP(c), FACP, FACE
Michelle Mackness, MC, Private Practice
Aaron Kimberley, LGBTCC Public Engagement Director
References
Abbruzzese, E., Levine, S. B., & Mason, J. W. (2023). The Myth of “Reliable Research” in Pediatric Gender Medicine: A critical evaluation of the Dutch Studies—and research that has followed. Journal of Sex & Marital Therapy, 1–27. https://doi.org/10.1080/0092623X.2022.2150346
Allen, L. R., Watson, L. B., Egan, A. M., & Moser, C. N. (2019). Well-being and suicidality among transgender youth after gender-affirming hormones. Clinical Practice in Pediatric Psychology, 7(3), 302–311. https://doi.org/10.1037/cpp0000288
Baker, K. E., Wilson, L. M., Sharma, R., Dukhanin, V., McArthur, K., & Robinson, K. A. (2021). Hormone Therapy, Mental Health, and Quality of Life Among Transgender People: A Systematic Review. Journal of the Endocrine Society, 5(4), bvab011. https://doi.org/10.1210/jendso/bvab011
Baxendale, S. (2024). The impact of suppressing puberty on neuropsychological function: A review. Acta Paediatrica, n/a(n/a). https://doi.org/10.1111/apa.17150
Biggs, M. (2020). Puberty Blockers and Suicidality in Adolescents Suffering from Gender Dysphoria. Archives of Sexual Behavior. https://doi.org/10.1007/s10508-020-01743-6
Biggs, M. (2021). Revisiting the effect of GnRH analogue treatment on bone mineral density in young adolescents with gender dysphoria. Journal of Pediatric Endocrinology and Metabolism. https://doi.org/10.1515/jpem-2021-0180
Biggs, M. (2022). Suicide by Clinic-Referred Transgender Adolescents in the United Kingdom. Archives of Sexual Behavior. https://doi.org/10.1007/s10508-022-02287-7
Block, J. (2023a). Gender dysphoria in young people is rising—And so is professional disagreement. BMJ, 380, p382. https://doi.org/10.1136/bmj.p382
Block, J. (2023b). Norway’s guidance on paediatric gender treatment is unsafe, says review. BMJ, 380, p697. https://doi.org/10.1136/bmj.p697
Coleman, E., Radix, A. E., Bouman, W. P., Brown, G. R., de Vries, A. L. C., Deutsch, M. B., Ettner, R., Fraser, L., Goodman, M., Green, J., Hancock, A. B., Johnson, T. W., Karasic, D. H., Knudson, G. A., Leibowitz, S. F., Meyer-Bahlburg, H. F. L., Monstrey, S. J., Motmans, J., Nahata, L., … Arcelus, J. (2022). Standards of Care for the Health of Transgender and Gender Diverse People, Version 8. International Journal of Transgender Health, 23(sup1), S1–S259. https://doi.org/10.1080/26895269.2022.2100644
Dahlen, S., Connolly, D., Arif, I., Junejo, M. H., Bewley, S., & Meads, C. (2021). International clinical practice guidelines for gender minority/trans people: Systematic review and quality assessment. BMJ Open, 11(4), e048943. https://doi.org/10.1136/bmjopen-2021-048943
de Graaf, N. M., Steensma, T. D., Carmichael, P., VanderLaan, D. P., Aitken, M., Cohen-Kettenis, P. T., de Vries, A. L. C., Kreukels, B. P. C., Wasserman, L., Wood, H., & Zucker, K. J. (2020). Suicidality in clinic-referred transgender adolescents. European Child & Adolescent Psychiatry. https://doi.org/10.1007/s00787-020-01663-9
Lane, B. (2024, February 5). Probe the protocol. Gender Clinic News. https://www.genderclinicnews.com/p/probe-the-protocol
Levine, S. B. (2019). Informed Consent for Transgendered Patients. Journal of Sex & Marital Therapy, 45(3), 218–229. https://doi.org/10.1080/0092623X.2018.1518885
Levine, S. B., Abbruzzese, E., & Mason, J. M. (2022). Reconsidering Informed Consent for Trans-Identified Children, Adolescents, and Young Adults. Journal of Sex & Marital Therapy, 48(7), 1–22. https://doi.org/10.1080/0092623X.2022.2046221
Martínez, V., Jiménez-Molina, Á., & Gerber, M. M. (2023). Social contagion, violence, and suicide among adolescents. Current Opinion in Psychiatry, 36(3), 237–242. https://doi.org/10.1097/YCO.0000000000000858
Mohamed, R. (2024, February 5). Nope, Alberta’s gender policy isn’t a matter of “life and death.” National Post. https://nationalpost.com/opinion/rahim-mohamed-nope-albertas-gender-policy-isnt-a-matter-of-life-and-death
National Institute for Health and Care Excellence. (2020). Evidence review: Gender-affirming hormones for children and adolescents with gender dysphoria. National Institute for Health and Care Excellence. https://cass.independent-review.uk/wp-content/uploads/2022/09/20220726_Evidence-review_Gender-affirming-hormones_For-upload_Final.pdf
Right Side of HistoryTM️ [@xxclusionary]. (2023, May 20). I got the book “Let’s Talk About It,” so you don’t have to. A Thread [Tweet]. Twitter. https://twitter.com/xxclusionary/status/1660035667387088898
SEGM. (2023, August 17). Denmark Joins the List of Countries Who Have Sharply Restricted Youth Gender Transitions. https://segm.org/Denmark-sharply-restricts-youth-gender-transitions
Singh, D., Bradley, S. J., & Zucker, K. J. (2021). A Follow-Up Study of Boys With Gender Identity Disorder. Frontiers in Psychiatry, 12. https://doi.org/10.3389/fpsyt.2021.632784
Sinyor, M., Schaffer, A., Heisel, M. J., Picard, A., Adamson, G., Cheung, C. P., Katz, L. Y., Jetly, R., & Sareen, J. (2018). Media Guidelines for Reporting on Suicide: 2017 Update of the Canadian Psychiatric Association Policy Paper. The Canadian Journal of Psychiatry, 63(3), 182–196. https://doi.org/10.1177/0706743717753147
SOGI 1 2 3 / Alberta. (n.d.). SOGI 1 2 3 / Alberta. Retrieved February 6, 2024, from https://ab.sogieducation.org
Sorbara, J. C., Chiniara, L. N., Thompson, S., & Palmert, M. R. (2020). Mental Health and Timing of Gender-Affirming Care. Pediatrics, 146(4). https://doi.org/10.1542/peds.2019-3600
Steensma, T. D., McGuire, J. K., Kreukels, B. P. C., Beekman, A. J., & Cohen-Kettenis, P. T. (2013). Factors Associated With Desistence and Persistence of Childhood Gender Dysphoria: A Quantitative Follow-Up Study. Journal of the American Academy of Child & Adolescent Psychiatry, 52(6), 582–590. https://doi.org/10.1016/j.jaac.2013.03.016
Stolk, T. H. R., Asseler, J. D., Huirne, J. A. F., van den Boogaard, E., & van Mello, N. M. (2023). Desire for children and fertility preservation in transgender and gender-diverse people: A systematic review. Best Practice & Research Clinical Obstetrics & Gynaecology, 87, 102312. https://doi.org/10.1016/j.bpobgyn.2023.102312
Turban, J. L., King, D., Carswell, J. M., & Keuroghlian, A. S. (2020). Pubertal Suppression for Transgender Youth and Risk of Suicidal Ideation. Pediatrics, 145(2), e20191725. https://doi.org/10.1542/peds.2019-1725
World Health Organization. (2024). Frequently Asked Questions (FAQ) WHO development of a guideline on the health of trans and gender diverse people. https://cdn.who.int/media/docs/default-source/hq-hiv-hepatitis-and-stis-library/tgd_faq_16012024.pdf?sfvrsn=79eaf57f_1
Wright, C. (2021, February 10). Sex Is Not a Spectrum. Reality’s Last Stand. https://www.realityslaststand.com/p/sex-is-not-a-spectrum

Excellent response to the pseudoscience of these organizations. WPATH is a very well-funded propaganda machine that has most certainly captured many well intentioned health care providers. There MUST be more open and measured discussion across medical, political and social divides to provide excellent care for our young people seeking real answers to the struggles they are undergoing. Creating lifelong medical patients only benefit drug companies and “some people’s” salaries. It will not save the lives of our children or young adults.
Please continue your very important work.
From a Lesbian Psychotherapist and activist in Nova Scotia.
A cogent and rational response. I love hearing people speak up for academic, intellectual honesty. Not being hyperbolic, for thousand years, we’ve used logic as a way to ascertain truth, and in the last five hundred, we’ve formalized a specialized form of it in what we call science.
So many thoughts and ideas in social issues are characterized by the emotions of the subject, thus so many thoughts and ideas in social issues are characterized by perception, by subjective reality. Now, I’ll get off my soap box to thank you for taking the time to put this cogent and rational response together for those of us that don’t have the words or the voice to do so.