UK Says NO to Routine Use of Puberty Blockers
Europe continues to change course and adopt a cautious stance towards medicalizing gender non-conforming youth. The UK’s National Health Service announced the public consultation phase for their new policy on the treatment options for children with gender incongruence. They issued this summary statement that provides clarity on the usage of puberty blockers from the UK NHS:
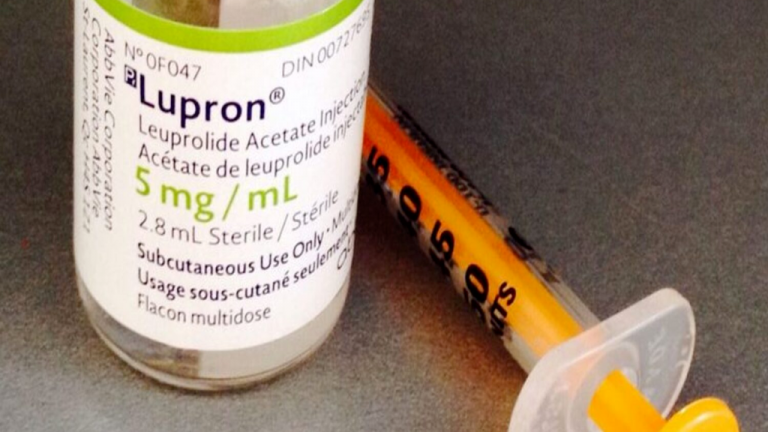
“The policy proposition is that puberty suppressing hormones are not recommended to be available as a routine commissioning option for the treatment of children and adolescents who have gender incongruence or dysphoria.”
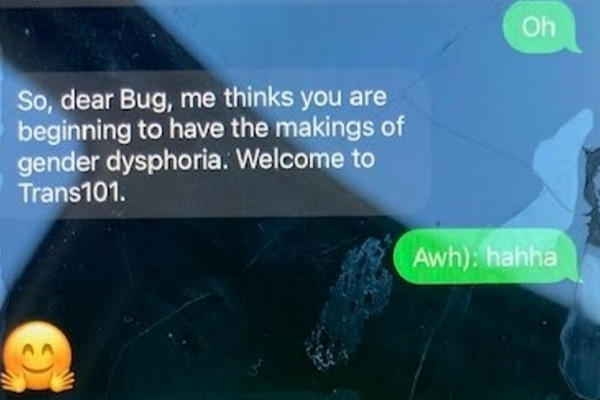
The UK Parliament also published a report this week “Factors shaping gender incongruence and gender dysphoria, and impact on health services”. It provides a very balanced review of factors that can contribute to gender-related distress, including peer influence that is impacting children and adolescents and cites rates of up to 30% detransition or people stopping medical treatments for various reasons.
Earlier this month, the Health Minister in Denmark announed that their specialized health system has “become reluctant” to offer medical gender transition for adolescents who did not present with the classic early-onset childhood GD due to the lack of evidence supporting these treatments and the National Health Board announced they would not support gender surgeries for under-18’s. This follows Sweden and Finland making formal changes and Norway making announcements that appear they are reconsidering their approach as well.
Will US Medical Societies Follow Suit?
The American Academy of Pediatricians (which also represents Canadian pediatricians) may be starting to cave to pressure to evaluate their recommendations for gender-affirmation care. They announced this week that they would undertake a systematic review of evidence and update their guidance.
At the same time, the AAP executive said they support “gender affirming care”. It’s a very mixed message and illustrates the group think that surrounds gender “affirmation”. Three systematic evidence reviews have already been done in Europe and the Florida Medical Board has done a “review of reviews”. The findings from the AAP will not change. We see the announcement as a ploy to buy some time as the AAP (hopefully) works out how they’re going to backpedal from the current policy they continue to promote.
Canadian research expert, Dr Gordon Guyatt of McMaster University was quoted in the New York Times yesterday saying the A.A.P.’s report will most likely find low-quality evidence for pediatric gender care. “The policies of the Europeans are much more aligned with the evidence than are the Americans’,” he said.
Ultimately, the findings of the evidence review will depend upon the inclusion and exclusion criteria used. It may be that the AAP wants to direct the systematic review in a different direction than the Europeans have done. It’s important that the AAP focuses on the issue of patient safety and whether treatments with puberty blockers, hormones and surgeries have evidence that the benefit of these treatments outweighs the risks. This is something to watch closely as the evidence review takes shape.
Canadian Gender Clinics Continue to Cite WPATH and Endocrine Society Guidelines
US Medical societies like the AAP have a significant influence in Canada. Most of our provinces are citing WPATH as the “standard of care”. Gender clinics will refer to “being aligned with WPATH and Endocrine Society guidelines” when parents file complaints about the lack of assessments being used to determine who may be a good candidate for puberty blockers.
Endocrine Society practice guidelines refer to the need for mental health assessments. These are being systematically phased out at Canadian clinics, which begs the question, exactly how are the Endocrine Society guidelines being used? Canadian hospitals and clinics refer to WPATH and Endocrine Society guidance to construe “expert consensus” support for their routine usage of puberty blockers and cross-sex hormones in children and young people presenting with gender incongruence.
WPATH influence on Endocrine Society Unacceptable
The Endocrine Society guidelines were developed by a group of individuals closely affiliated with WPATH. 9/10 are WPATH members or worked on WPATH’s scientific committee. 7 are WPATH leadership and only 1 member has no known WPATH affiliation. This is clearly not an independent group of endocrinologists who are looking at the evidence objectively because WPATH has significant bias and their consensus approach to establishing its guidelines has silenced debate and dissenting views.
Endocrine Treatment of Gender-Dysphoric/Gender-Incongruent Persons: An Endocrine Society* Clinical Practice Guideline
Wylie C Hembree, Peggy T Cohen-Kettenis, Louis Gooren, Sabine E Hannema, Walter J Meyer,
M Hassan Murad, Stephen M Rosenthal, Joshua D Safer, Vin Tangpricha, Guy G T’Sjoen
https://academic.oup.com/jcem/article/102/11/3869/4157558
Authors’ WPATH role
Wylie Hembree – On scientific committee for WPATH 2009 XXI Biennial symposium
Peggy Cohen-Kettenis – WPATH Board of Directors 1995-1999
Louis Gooren – WPATH Board of Directors 1999-2003
Sabine E. Hannema – WPATH member
Walter J. Meyer – WPATH President 2003-2005
M. Hassan Murad – not found as WPATH member
Stephen M. Rosenthal – WPATH Board of Directors – (Members-at-large) 2020-2024
Joshua D. Safer – serves on WPATH’s global education initiative committee and on WPATH’s standards of care revision committee
Vin Tangpricha – WPATH president elect 2017, standards of care revision committee
Guy G. T’Sjoen – WPATH Board of Directors – (Members-at-large) EPATH representative 2020-2022
Patient Safety must be the priority
Medical societies must be able to substantiate their guidance in this highly contentious area of medical practice. Guidance from the AAP and the Endocrine Society is being used to support the routine use of puberty blockers and cross-sex hormones for children and young people presenting with gender incongruence. Recent Canadian research revealed that 62% of clinics offer hormonal interventions at the first visit. This number isn’t higher simply because (as the study calls out) it’s the stated practice of these other clinics NOT to offer hormones at the first visit. Further, this exposes how mental health assessments are being phased out and replaced with an “affirmation” approach that does not allow assessments that question or explore whether hormonal interventions are in a young person’s long-term best interest.
Medical societies cannot simply wash their hands of this reality. The lack of caution being exercised by medical practitioners in the routine prescribing of hormonal interventions for gender-incongruent youth is a concern as thousands of mostly adolescent women flock to these treatments. Patient safety needs to be the priority and practice guidelines must be re-evaluated with this lens.



Wonderful web site Lots of useful info here Im sending it to a few friends ans additionally sharing in delicious And obviously thanks to your effort